Despite the recession, Oregon expands health coverage with federal help
By Janet Bauer
Oregon is making strides in helping Oregonians get health coverage, a remarkable development considering that the recent economic recession wreaked havoc on the state’s finances. Since 2009, Oregon has been carrying out a plan to provide health insurance for previously uninsured children and adults by bolstering existing medical assistance programs and public-private health partnerships.
As of June 2011, Oregon exceeded its Oregon Health Plan enrollment goals for children and adults with few earnings. The progress in children’s coverage is especially fortuitous, given that the federal government has rewarded the state with additional federal dollars because of the achievement.
This issue brief describes Oregon’s success in improving coverage among uninsured Oregonians and how state and federal policymakers enabled the accomplishment despite difficult economic circumstances.
Download a copy of the issue brief:
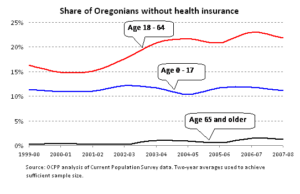
Health coverage woes deepened during the just-concluded decade
In the opening years of the new millennium, the gap in health coverage among Oregonians remained a festering wound. In the years 1999 to 2008, about 11 percent of Oregon’s children had no insurance. The rate among working-age adults jumped from 16 percent to 22 percent over the period. By the time the legislature convened in 2009, some 97,000 children and 524,000 working-age adults had no health insurance. The only bright spot was coverage for people age 65 and older, nearly all of whom were insured through Medicare, retiree coverage or veterans’ benefits.
The lack of health insurance exacted a heavy toll on those exposed. In 2007, for example, 71 percent of uninsured American adults reported that they had gone without needed health care. Forty-two percent of Americans reported delaying or going without routine preventive care and 60 percent reported having problems with medical debt.[1]
The lack of health insurance also put pressure on Oregon’s health care infrastructure. In 2007, Oregon hospitals — institutions that cannot turn away the uninsured who come to their emergency rooms — wrote off $223 million more in consumer medical debt than they did in 2000, a 173 percent increase. [2]
The decline in health insurance among working-age Oregonians reflected a trend in fewer getting coverage through their workplace. In the 1999-2000 period, 69 percent of working-age Oregonians were insured through an employer. By 2007-08, that share had fallen to 63 percent.[3]
It wasn’t just employment-based coverage that shrank during this period.
The Oregon Health Plan (OHP), an ambitious program launched in 1994 to extend Medicaid coverage to poor Oregonians not receiving public assistance, also experienced a sharp decline in the number of those covered. At its peak in 1995, OHP covered over 130,000 poor adults who would not otherwise have qualified for Medicaid, which under federal rules must cover the aged, blind, disabled, low-income pregnant women and recipients of cash assistance.[4] Unfortunately, subsequent cuts in the 1990s shed thousands from the program. Then a recession in 2001 dramatically reduced state revenues. The legislature responded by separating the expanded pool of adult beneficiaries into a program called OHP Standard, with reduced benefits compared to those in OHP Plus, the new name for the part of OHP covering those who otherwise qualified under federal Medicaid rules.
Then in 2003, under continued revenue pressure, the state again slashed support for OHP Standard, causing enrollment to plummet. The state closed OHP Standard to new enrollees in 2004. Due to attrition, enrollment dwindled to fewer than 18,000 by 2008.[5]
At the time legislature convened in 2009, Oregon’s efforts to provide health coverage to the uninsured outside the Oregon Health Plan were important but modest, in view of the more than half a million Oregonians lacking insurance. For instance, through its Family Health Insurance Assistance Program (FHIAP), the state was helping some low-income Oregonians obtain private insurance coverage, coverage that would otherwise have been unaffordable. In 2008, FHIAP helped 13,000 low-income families secure coverage by contributing to individual or group health insurance premiums. [6] Federal Medicaid and state dollars went toward these premium subsidies. Additionally, a “high-risk” insurance pool, the Oregon Medical Insurance Pool (OMIP), where premiums were subsidized by Oregon’s insurers, helped 15,000 Oregonians who had been rejected for individual coverage due to a pre-existing condition.[7]
By 2009, a few other programs also provided some health coverage. As required by federal law, the state provided emergency medical insurance for low-income, legal residents who weren’t eligible for OHP — a program that assisted 17,500 Oregonians in 2008. The state also assisted some low-income Medicare enrollees with expenses that Medicare didn’t pay for and helped some low-income women get breast and cervical cancer screening and treatment.[8]
Toward the end of the decade, as the Great Recession engulfed the state and the nation, prospects for improving health insurance coverage in Oregon looked grim.
The 2009 Oregon legislature expands health coverage
The growing health coverage problem did not go unnoticed by the 2009 Oregon legislature, which took two important steps to address it. First, it enacted the Healthy Kids program to cover nearly all of Oregon’s uninsured children. Second, it opened the Oregon Health Plan to more poor uninsured adults.
To pay for the coverage expansions for children and poor adults, the legislature enacted new taxes on hospitals and insurers. House Bill 2116 established a 1 percent assessment on insurance premiums and on the per-person Medicaid payments provided by the state to Medicaid managed care organizations.[9] It also reinstated and expanded hospital assessments, a tax on net profits. With these actions, the state expected to generate $359 million in new revenue during the 2009-11 biennium, money that was expected to leverage an additional $768 million in federal Medicaid matching dollars.[10]
Expanded coverage for children
The new Healthy Kids program expanded and improved existing public health insurance structures. It opened the Oregon Health Plan to children with income up to 200 percent of the federal poverty line (set at $44,700 for a family of four in 2011), where before it only covered children with income up to 185 percent of poverty ($41,348 for a family of four in 2011).[11] The plan also streamlined enrollment, making it easier for families to get coverage for their kids.
For children who were not eligible for OHP, Healthy Kids aimed to make available affordable health coverage through a “Healthy KidsConnect” marketplace. Participating insurance companies were not permitted to discriminate against children with pre-existing health conditions by denying them coverage or charging them more than they would healthier children. Plans had to provide a comprehensive package of benefits. Families with income up to 300 percent of the federal poverty level received state assistance with premium costs on a sliding scale basis. By requiring insurers to provide quality coverage to all comers, the program aimed to encourage healthy children to enroll. If successful, the approach would lower the cost per child for insurers and thereby make premiums more affordable.
In relatively short order, Healthy Kids made substantial progress in covering Oregon’s uninsured children. Healthy Kids enrolled 93,892 children between July 2009 and June 2011, a number that exceeded the goal of 80,000 additional kids covered. Among the newly-insured, 88,802 were from families with income at or below 200 percent of the federal poverty line. Another 5,196 enrolled in the private Healthy KidsConnect program, most of whom received help with premium costs.[12] The marked progress in enrollment followed an aggressive promotional effort by the state.
The federal government rewarded the state for its gains in child coverage by providing a “performance bonus” of $15 million in December 2010.
It’s too soon to know the effect of Healthy Kids in reducing the share of Oregon children without coverage.[13] U.S. Census American Community Survey data for 2010, to be released in the fall of 2011, may very well show improvement given the significant enrollment success.
Expanded coverage for adults with poverty-level income
After several years of keeping its doors shut, OHP Standard reopened in 2008. Enrollment in the program had fallen below the budgeted level of 24,000, allowing the Department of Human Services (DHS) to begin offering coverage to uninsured adults with poverty-level income not qualifying for OHP Plus. DHS invited Oregonians who thought they might qualify to place their names on a registry from which the agency would periodically randomly select individuals to invite to apply for OHP Standard coverage.
The following year, OHP received a funding boost from the hospital assessment. With these resources the state set a goal of increasing OHP Standard enrollment to 60,000 by June 30, 2011 — more than doubling its 2008 limit. DHS began soliciting more names for the registry and holding frequent drawings of registrants. As of June 2011, the state enrolled 70,347 people, more than the targeted number of individuals, advancing the legislative goal of reaching more uninsured poverty-level adults in need.[14]
It’s too soon to tell what impact the OHP Standard expansion is having on the rate of adult Oregonians without health insurance.[15] However, the fact that the plan reopened its doors and more than doubled its participation level can only help Oregon stem the rising tide of the uninsured.
The 2009 Recovery Act rewards Oregon’s health coverage initiative
As bold as Oregon’s legislative actions were in 2009, they were unlikely to have resulted in forward motion without congressional enactment of the American Recovery and Reinvestment Act of 2009 (“Recovery Act”). The economic downturn, which turned out to be far more severe than experts had predicted, dug a hole in the state budget much larger than the new revenues generated by HB 2116 could fill. Oregon’s initiative in raising new revenue for expanded health coverage, however, enabled the state to leverage more federal health care dollars than it would have without the new revenue.
Congress understood that the recession would exacerbate the nation’s health coverage crisis. The recession intensified the loss of employer-based coverage as the economy shed jobs and pressured employers to cut costs. And at a time when employer-based coverage declined, the recession would shrink state revenues and curtail the ability of state health programs to simply maintain existing coverage levels, much less to respond to the rising need.
Congress also recognized the effectiveness of federal health care dollars in stabilizing the economy. According to Mark Zandi, Chief Economist of Moody’s Economy.com, state and local fiscal relief (primarily increased Medicaid and education funding) were estimated to generate $1.41 worth of economic activity for every dollar invested.[16] Medicaid dollars reach all corners of the state, flowing mainly to private-sector health clinics, hospitals, pharmacies and other health-related facilities.
The health care dollars Oregon received from the Recovery Act proved significant. Oregon received $454 million in extra Medicaid funds for the 2009-11 biennium — more than all of the projected new hospital and insurance tax revenues for the period. The Recovery Act dollars going to children and families in OHP programs — $397 million — more than tripled the amount these programs received from HB 2116. In the case of the FHIAP premium subsidy program, the dollars from the Recovery Act matched the amount coming from the revenue generated by the new state tax on insurers: $3.8 million. The Recovery Act also contributed $51.4 million to OHP Standard, an amount equivalent to about 30 percent of the funds coming from the new state tax on hospitals.[17]
Federal Medicaid funds, including the additional funds provided through the Recovery Act, aren’t a handout to states. States earn the federal funds only by spending their own dollars. The structure of the federal Medicaid program rewards states for investing their own resources to cover the most vulnerable by matching the state dollars at favorable match rates. Many states, including Oregon, receive more in federal Medicaid dollars than they spend from their own coffers.
Seeking Savings Without Going Back on Enrollment Gains
The 2011 Oregon Legislature enacted legislation intended to reduce state health care spending and improve people’s health, without taking a step backward in Oregon’s enrollment gains. HB 3650 aims to make health care more efficient and effective by rewarding providers for coordinating physical, mental and oral health care, emphasizing prevention and effectively managing chronic diseases among people in the Oregon Health Plan and low-income Medicare recipients.
HB 3650 enacts a key piece of reform sought by Gov. John Kitzhaber, who expressed his opposition to extracting savings by reducing health care coverage as a way to address the increasing cost of health care:
What I am putting before the legislature is a proposal to address this problem by fundamentally changing our heath care delivery system to improve the health of the population, at a lower cost while improving the patient experience in terms of clinical outcomes, patient safety and patient satisfaction.
Unlike the short-sighted decisions of other states that are considering dropping Medicaid recipients from state coverage, we’re taking a different approach – because there’s nothing to gain and a lot to lose by stripping people of coverage, only to have them show up in emergency rooms – where we end up treating their stroke in the hospital rather than managing their high blood pressure in the community.[18]
The share of federal dollars in Oregon’s Medicaid program, which otherwise would have been about 62.5 percent over the biennium, increased to 73 percent due to the Recovery Act’s enhanced match rates.[19] That meant that on average Oregon received $73 from the federal government for every $27 it spent of its own resources to cover uninsured, low-income Oregonians during the 2009-11 period.
Preserving and strengthening Medicaid-funded programs such as OHP and FHIAP during the recession proved a smart move for Oregon. Fortunately, Oregon capitalized on an opportunity to attract substantial additional federal dollars, funds that helped the state weather the storm.
Conclusion
Against economic headwinds whipped up by the Great Recession, Oregon took action to address distressing levels of lack of health insurance among its residents. The 2009 legislature raised new revenue to help meet the deepening need. Fortunately, Congress had responded to the economic crisis by temporarily boosting federal investments in Medicaid. With the additional federal funds and new state dollars, Oregon was able to cover more uninsured children and reopen doors to the Oregon Health Plan for low-income adults.
[1] Sara R. Collins, Jennifer L. Kriss, Michelle M. Doty and Sheila D. Rustigi, Losing Ground: How the Loss of Adequate Health Insurance is Burdening Working Families, Commonwealth Fund Biennial Health Insurance Surveys, 2001-2007, Commonwealth Fund, August 2008.
[2] Michael Leachman and Joy Margheim, Rolling Up Our Sleeves: Building an Oregon That Works for Working Families, the State of Working Oregon 2008-2009, Oregon Center Public Policy, December 2008.
[3] OCPP analysis of U.S. Census, Current Population Survey (CPS) data. Two-year data used to achieve sufficient sample size.
[4] Under federal rules, state Medicaid programs must cover pregnant women and children under the age of 6 with income below 133 percent of the federal poverty level (FPL); children ages 6 to 18 with income below 100 percent of FPL; foster children with income less than 46 percent of FPL; families receiving cash assistance in Oregon’s TANF program; individuals who are blind or disabled and seniors with income under 100 percent of the SSI income level; and individuals who are blind or disabled and seniors who meet certain long-term care criteria and have income up to 300 percent of the SSI income level.
[5] The low point for Oregon Health Plan Standard during the decade was 17,576 covered individuals in March 2008, according to Oregon Department of Human Services enrollment reports.
[6] FHIAP caseload figure for November 2008 from Oregon Office of Health Policy and Research, Trends in Oregon’s Health Care Market and the Oregon Health Plan, A Report to the 75th Legislative Assembly, February 2009. The income threshold for FHIAP was 185 percent of the federal poverty level.
[7] Oregon Office for Health Policy and Research, Trends in Oregon’s Health Care Market and the Oregon Health Plan, A Report to the 75th Legislative Assembly, February 2009, pp. 65-55. Also, Oregon Medical Insurance Pool Stat Pack, November 2010. In November, 2008, 15,343 individuals received coverage through the OMIP program. This figure includes 1,684 individuals getting a Medicaid premium subsidy through the FHIAP program, 864 people getting assistance with HIV drugs supported by the federal CAREAssist program and 44 individuals getting premium assistance under the federal Health Care Tax Credit program. Subsidies to others getting coverage through OMIP were supported by an assessment on licensed insurers.
[8] Oregon provided emergency medical services to 17,517 legal resident aliens in October 2008 through its Citizen Alien-Waived Emergency Medical (CAWEM) program. The state provided assistance with Part B premiums, and in some cases, with out-of-pocket costs, to Medicare beneficiaries with low income through its Qualified Medicare Beneficiary (QMB) program. It also provided breast and cervical cancer screening and treatment to middle-aged women with modest income who hadn’t had recent screenings and who didn’t have access to such services through a health insurance plan, through its Breast and Cervical Cancer Program (BCCP). The QMB and the BCCP together served 13,715 Oregonians in October 2008. BCCP receives funds from the federal Centers for Disease Control and Prevention and the Susan G. Komen for the Cure of Oregon and SW Washington Affiliate. Data obtained from Oregon Department of Human Services eligibility reports.
[9] HB 2116 established a 1 percent assessment on premiums collected by insurers and a 1 percent assessment on capitation payments (a fixed amount per member covered paid to an insurer) received by Medicaid managed care organizations from Oregon’s medical assistance programs, including the Oregon Health Plan.
[10] 75th Oregon Legislative Assembly – 2009 Regular Session, Budget Report and Measure Summary, Joint Committee on Ways and Means, SB 5529-A, page 3.
[11] OHP uses federal Medicaid matching funds to cover children ages zero to 5 with family income up to 133 percent of the federal poverty level and children ages 6 to 18 up to 100 percent of the poverty level. In addition, prior to 2009, OHP used federal State Children’s Health Insurance Program (CHIP) matching dollars to cover children above its Medicaid income limits up to 185 percent of the federal poverty level. With approval of HB 2116 in 2009, Oregon now uses federal CHIP matching funds to cover children above Medicaid eligibility levels up to 200 percent of the federal poverty level.
[12] Of the newly enrolled 93,892 children, 88,802 were enrolled in the Oregon Health Plan, 5,196 were enrolled in Healthy KidsConnect and 106 had dropped from the FHIAP program since June 2009. Data emailed by Oregon Health Authority staff, Loralyn Spiro, to author on July 14, 2011. Healthy KidsConnect subsidy information provided by email from Anna Holowetzki, Oregon Health Policy and Research, July 15, 2011.
[13] Although the Oregon Health Authority (OHA) recently claimed that the rate of Oregon children who were uninsured fell from 11.3 percent in 2009 to 5.6 percent in 2011 (see OHA, “New survey results show Oregon has reduced by half the number of uninsured children,” July 11, 2011), OHA acknowledges that “[e]stimates from 2009 and 2011 are not directly comparable because different survey methodologies were employed.” See OHA, 2011 Oregon Health Insurance Survey: Initial results. OHA used U.S. Census American Community Survey data for its 2009 estimates and the new Oregon Health Insurance Survey (OHIS) data for its 2011 estimate. The fall 2011 release of new U.S. Census American Community Survey data will provide comparable data.
[14] Data from DHS enrollment report showing census as of June 15, 2011. According to email communication on January 28, 2011 from DHS to author, the state is able to cover slightly more individuals in OHP Standard through the end of the 2009-11 biennium than originally anticipated because ramp-up of the expansion was somewhat slower than anticipated. The slower initial enrollment created fewer outlays in the early months of the biennium than expected, making extra dollars available in the latter months of the biennium.
[15] As noted in endnote 13, the new Oregon Health Insurance Survey cannot be used to estimate whether there has been improvement in the uninsurance rate among working Oregonians. U.S. Census American Community Survey data from 2010 that will be released in the fall of 2011 will provide some insight.
[16] Mark Zandi, The Impact of the Recovery Act on Economic Growth, written testimony to the congressional Joint Economic Committee, October 29, 2009.
[17] Figures from email communication with Oregon Department of Human Services, December 12, 2010. $3.815 million in ARRA funds were used to support the FHIAP program. $3.785 million in new state insurer tax revenues supported the program.
[18] John Kitzhaber, Speech to City Club of Portland, March 4, 2011.
[19] Without the Recovery Act provisions, the federal Medicaid match rate for Oregon in 2009 would have been 62.45 percent. It would have been 62.74 percent in 2010.
Posted in Health Care.
More about: health insurance, healthy kids, medicaid, oregon health plan, recovery act